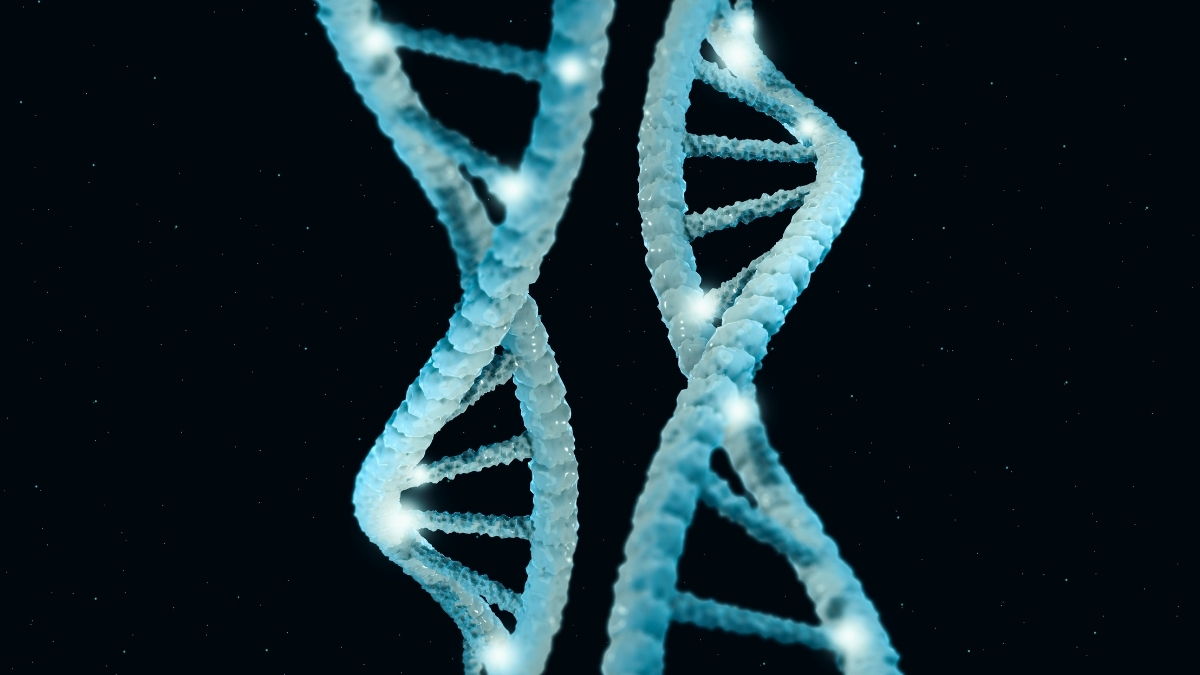
Research from the Centre National de la Recherche Scientifique (CNRS) in France has unveiled that unique proteins derived from camels and llamas, known as nanobodies, could play a crucial role in protecting the brain against Alzheimer’s disease and other challenging conditions. These nanoscopic proteins are capable of penetrating cellular spaces more effectively than traditional antibodies, offering potential breakthroughs in treatment options.
Scientists have found that the small size of these nanobodies allows them to navigate biological barriers, such as the blood-brain barrier, which often obstructs conventional drugs from reaching their targets in the brain. In recent studies, engineered nanobodies have demonstrated the ability to cross this barrier, targeting and eliminating key markers associated with Alzheimer’s, specifically tau and amyloid beta proteins.
Advancements in Nanobody Research
According to Philippe Rondard, a neuropharmacologist at CNRS, “Camelid nanobodies open a new era of biologic therapies for brain disorders and revolutionize our thinking about therapeutics.” The researchers believe these proteins could form a new class of drugs that bridge the gap between traditional antibodies and small-molecule drugs, which often have significant limitations in terms of bioavailability and side effects.
Historically, nanobodies have shown promise in treating various ailments, including influenza A and B, norovirus, COVID-19, and even HIV. Until recently, their application in brain disorders was limited due to the human kidneys’ rapid elimination of these proteins from the bloodstream. Additionally, there were concerns regarding their ability to traverse the blood-brain barrier, a critical requirement for effective brain-targeting treatments.
New animal model experiments have provided evidence that these engineered nanobodies can successfully cross the blood-brain barrier, presenting a significant advancement in therapeutic approaches to Alzheimer’s disease.
Future Steps for Clinical Application
Despite these promising findings, significant work remains before these therapies can be considered for human use. Prior to clinical application, scientists must assess the stability and proper folding of these nanobodies, as well as ensure they do not aggregate. “These are highly soluble small proteins that can enter the brain passively,” noted Pierre-André Lafon, a functional genomicist at CNRS. This characteristic contrasts with small-molecule drugs, which tend to be hydrophobic and often result in off-target interactions and increased side effects.
Further research is necessary to understand how long these nanobodies persist in the brain and the optimal dosages required for effective treatment. Developing stable formulations that can withstand long-term storage and transport is also a critical step in bringing these promising therapies from the laboratory to clinical settings.
The insights gained from this research, published in Trends in Pharmacological Sciences, highlight the potential for nanobody therapies to transform the landscape of treatment for Alzheimer’s disease. As scientists continue to explore the capabilities of these unique proteins, there is hope that one day, they may significantly impact the lives of those affected by neurodegenerative conditions.