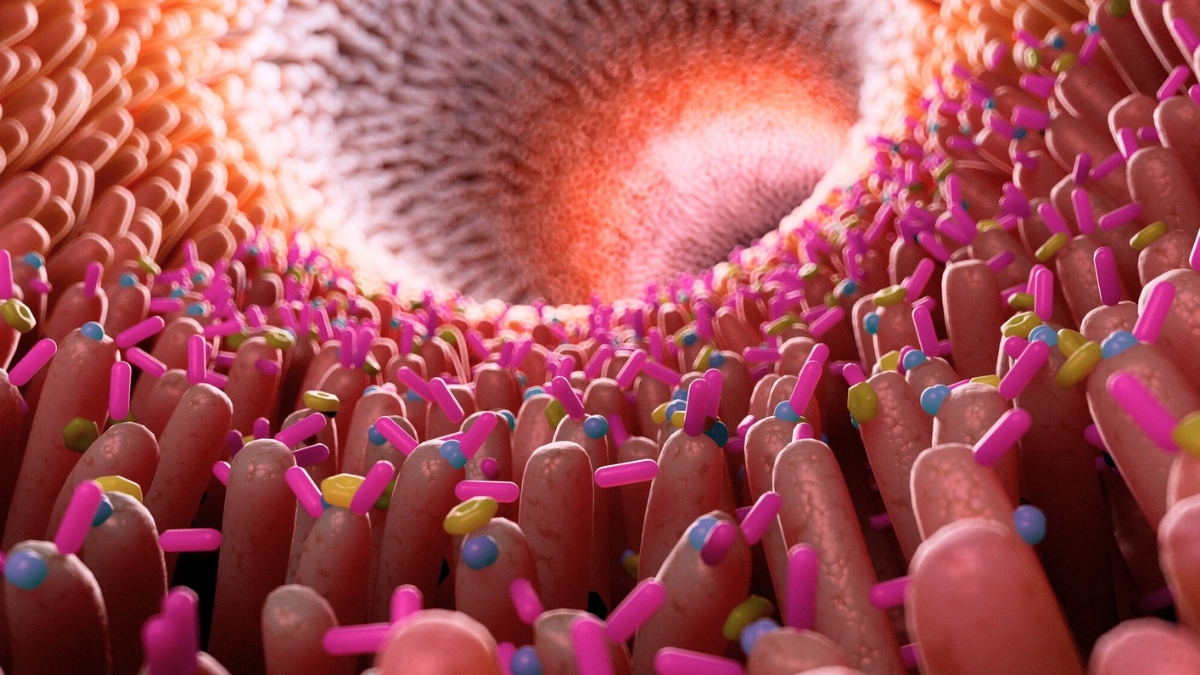
A new study has confirmed a significant link between gut inflammation and Alzheimer’s disease, adding to the understanding of this complex neurodegenerative condition. Researchers at the University of Wisconsin discovered that inflammation in the gut may serve as a mechanism connecting digestive health to brain health.
Animal studies have previously suggested that Alzheimer’s can be transmitted to young mice through gut microbes. This 2023 research expands on that theory, showing that individuals with Alzheimer’s have increased levels of gut inflammation. According to psychologist Barbara Bendlin, “We showed people with Alzheimer’s disease have more gut inflammation,” highlighting a correlation between inflammation and brain health.
To gather data, pathologist Margo Heston and her international team analyzed stool samples from 125 individuals involved in two Alzheimer’s prevention cohort studies. Participants underwent cognitive tests and interviews regarding family history and genetic risk factors for Alzheimer’s. Notably, a subgroup of participants was tested for the presence of amyloid protein clumps, which indicate the onset of the disease.
The findings revealed that levels of calprotectin, a marker of inflammation, were significantly elevated in older patients, particularly those exhibiting Alzheimer’s-related amyloid plaques. Additionally, as calprotectin levels rose, so did other Alzheimer’s biomarkers, while memory test scores declined. Even among participants without a formal Alzheimer’s diagnosis, higher calprotectin levels correlated with poorer memory performance.
While this study establishes important associations, Heston cautioned, “We can’t infer causality from this study; for that, we need to do animal studies.” Previous laboratory analyses indicated that chemicals produced by gut bacteria can initiate inflammatory responses in the brain. Other research has also recorded increased gut inflammation in Alzheimer’s patients compared to control groups.
The researchers propose that changes in the microbiome may lead to gut alterations, resulting in chronic yet mild inflammation. Federico Rey, a bacteriologist at the University of Wisconsin, explained, “Increased gut permeability could result in higher blood levels of inflammatory molecules and toxins derived from gut lumen, leading to systemic inflammation.” Such conditions could weaken the blood-brain barrier, potentially leading to neuroinflammation and subsequent neural damage.
To further investigate the implications of these findings, the research team is now testing whether specific dietary changes that elevate inflammation can induce Alzheimer’s symptoms in mice. Despite decades of research, effective treatments for Alzheimer’s remain elusive. However, this ongoing research brings scientists closer to unveiling the underlying biological processes of the disease.
The study has been published in Scientific Reports, and it marks another step in the intricate puzzle of understanding Alzheimer’s disease. As researchers piece together these findings, they hope to pave the way for improved prevention and treatment strategies for the millions affected by this condition worldwide.