A recent study has revealed that a common protein in human blood, known as albumin, can significantly influence the behavior of the yeast *Candida albicans*, transforming it from a harmless organism into a potentially dangerous pathogen. Researchers from Europe, including microbiologists from the Leibniz Institute for Natural Product Research and Infection Biology – Hans Knöll Institute, have found that albumin enhances the virulence of this fungus, shedding light on why it is difficult to study outside of the human body.
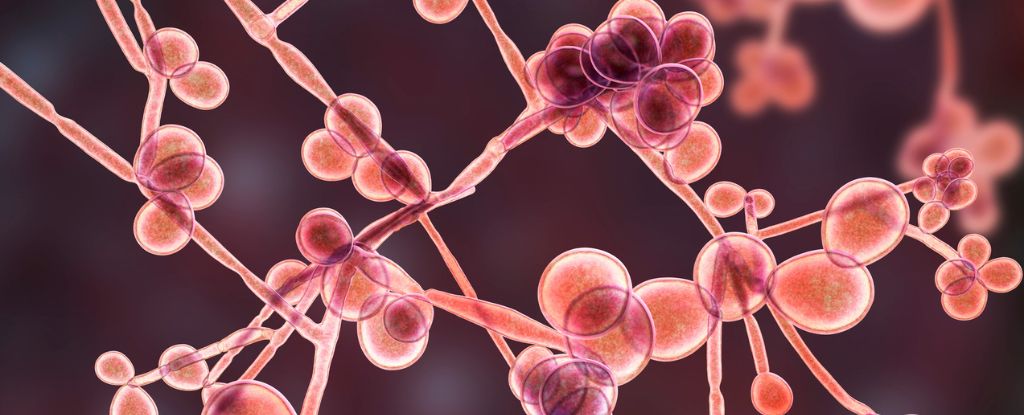
*Candida albicans* is typically found in benign states within the human population, residing in areas such as the mouth, gut, and genitals. However, under certain circumstances—such as when the immune system is compromised or following antibiotic treatments—this opportunistic pathogen can become aggressive, leading to conditions such as thrush and, in extreme cases, bloodstream infections that can invade organs.
The study emphasizes the duplicitous nature of *C. albicans*, which can appear non-virulent when isolated in laboratory conditions. According to Dr. Sophia Hitzler, a microbiologist involved in the research, this discrepancy raised questions about potential signals from the host that could be missing from test systems. The team hypothesized that albumin could be one such factor, as previous research indicated its role in enhancing the toxicity of *C. albicans* on human cells.
In the latest experiments, the research team, which included Dr. Candela Fernández-Fernández, focused on human cell models derived from the vulva. They discovered that albumin acted as a negative influence, stimulating *C. albicans* to rewire its metabolism, increasing its toxicity to human skin cells. The yeast not only became more harmful but also displayed accelerated growth, forming dense biofilms—a characteristic behavior of pathogenic organisms.
Even when researchers removed certain virulence genes from the yeast, the presence of human albumin restored its capacity to damage human cells. Dr. Fernández-Fernández noted that the fungus does not need to grow in a traditional manner to cause infection; it adapts to its environment and can exploit the host’s resources.
The implications of this research suggest that future investigations into fungal infections must take into account the complexities of the host’s physiology. Dr. Hitzler remarked, “Just providing essential nutrients in the lab is not enough. You need the right environmental cues. Otherwise, you might overlook strains that are actually dangerous in the human body.”
The World Health Organization has classified *C. albicans* as one of the most hazardous fungal infections globally. Despite the rising threat of fungal infections and their potential to develop resistance to medications, they receive considerably less scientific scrutiny compared to bacterial infections. To bridge this gap, accurately assessing the toxicity of fungi in laboratory settings is essential.
This study adds to the growing body of research exploring the intricate relationship between human physiology and microbial behavior. Published in *Nature Communications*, the findings highlight the need for a deeper understanding of how host factors influence pathogenicity, which could ultimately lead to more effective treatments for fungal infections.