A recent study has revealed a concerning rise in drug-resistant infections, commonly known as superbugs, in newborns across Southeast Asia. This research highlights the critical issue of antibiotic resistance, which has become one of the leading causes of death globally. In 2019, antibiotic resistance was responsible for an estimated 5 million deaths, surpassing mortality rates from HIV/AIDS and malaria. The new findings indicate that frontline treatments for conditions like sepsis may no longer be effective against most bacterial infections in newborns.
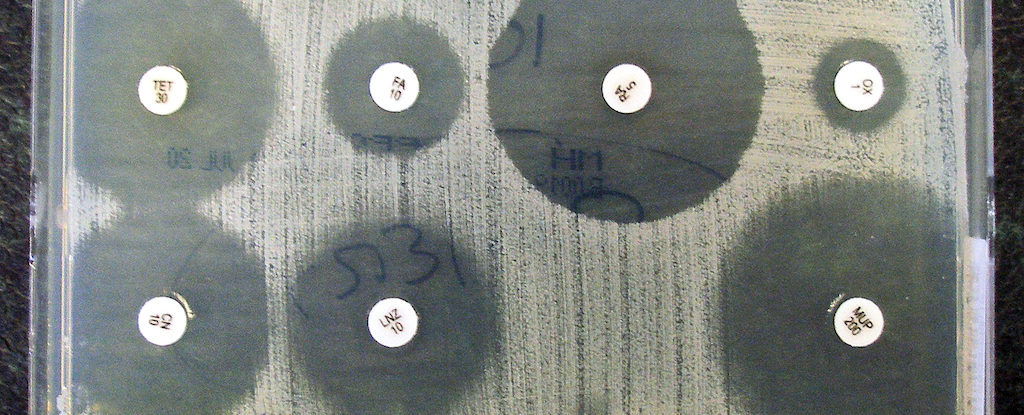
Researchers conducted the study between 2019 and 2020, analyzing nearly 15,000 blood samples collected from ill infants at ten hospitals across five countries in Southeast Asia. The investigation revealed that many infections were caused by bacteria resistant to standard antibiotics recommended by the World Health Organization (WHO) for treating neonatal sepsis.
Widespread Antimicrobial Resistance
The study illustrates a troubling prevalence of antimicrobial resistance (AMR) among disease-causing bacteria. According to Phoebe Williams, a pediatrician at the University of Sydney and co-author of the study, “Our study highlights the causes of serious infections in babies in countries across Southeast Asia with high rates of neonatal sepsis, and reveals an alarming burden of AMR that renders many currently available therapies ineffective for newborns.” Williams emphasizes the urgent need to update treatment guidelines to reflect local bacterial profiles and resistance patterns, warning that without such changes, mortality rates will likely continue to rise.
Co-author Michelle Harrison, a PhD candidate at the University of Sydney School of Public Health, noted that the lack of new antibiotics specifically developed for infants exacerbates the situation. “It takes about 10 years for a new antibiotic to be trialed and approved for babies,” Harrison explained. “With so few new drug candidates available, significant investment in antibiotic development is essential.”
The study found that a significant portion of infections in newborns was caused by Gram-negative bacteria, which have an inherent resistance to certain antibiotics. The most commonly identified bacteria included E. coli, Klebsiella, and Acinetobacter, accounting for nearly 80 percent of the infections studied. Williams remarked, “These bugs have long been considered to only cause infections in older babies, but are now infecting babies in their first days of life.”
The Need for Localized Data
The urgency of neonatal sepsis often prevents timely laboratory testing to identify the specific bacteria responsible, leading doctors to make informed guesses based on existing research. Unfortunately, much of this research is derived from high-income countries, which limits its applicability in regions with different bacterial profiles.
“The findings emphasize the necessity for more localized surveillance to guide treatment decisions,” Harrison stated. “Otherwise, we risk reversing decades of progress in reducing child mortality rates.” The study also highlighted that fungal infections accounted for nearly 10 percent of serious infections in newborns, a figure notably higher than in high-income countries.
Harrison concluded, “We need to ensure doctors are prescribing treatments that have the best chance of saving a baby’s life.” The implications of this study are profound, underscoring the urgent need for a coordinated global response to combat antibiotic resistance, particularly in vulnerable populations such as newborns.
The full study is published in the Lancet Regional Health – Western Pacific, providing a crucial insight into the growing challenge of antibiotic resistance in neonatal care.






