Groundbreaking research has led to the development of the first 3D-printed artificial mini-placentas, providing a novel approach to studying pregnancy complications. Published in Nature Communications, this study aims to unravel the complexities of placental development and address conditions such as preeclampsia that affect millions of pregnancies each year.
The placenta is a unique organ essential for fetal growth, expanding rapidly during pregnancy. However, studying this organ presents significant challenges. Traditional methods of obtaining placental samples can introduce risks of infection or miscarriage, while the tissue obtained after birth differs substantially from its early development phase. Animal models, often used in research, do not accurately represent human placental physiology, leaving a gap in understanding critical early stages of development.
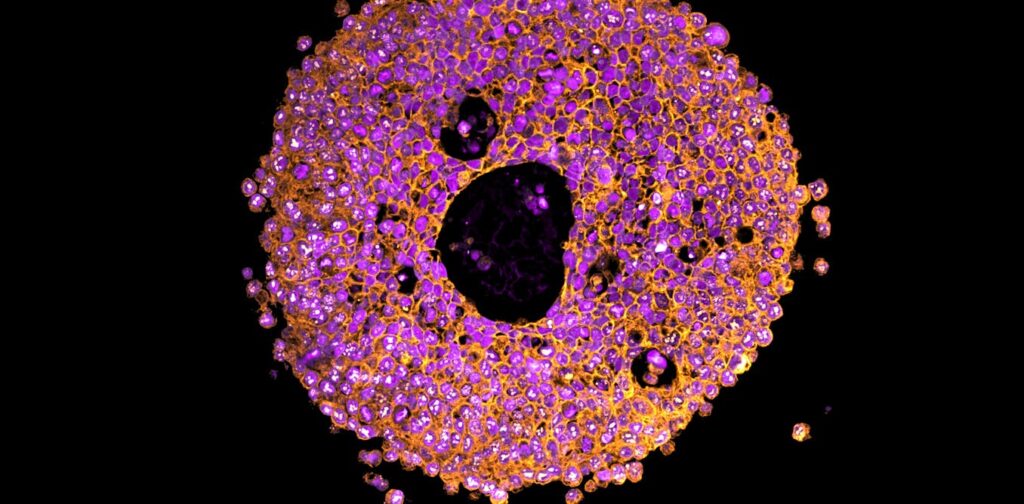
Researchers have turned to placental organoids—miniature, simplified versions of the organ—first successfully created from trophoblast cells in 2018. These organoids have facilitated insights into early pregnancy processes; however, they were primarily reliant on animal-derived gels that limited their application. The new bioprinting technology allows for greater precision and control, enabling scientists to create organoids in a more human-like environment.
Advancements in Bioprinting Technology
Utilizing a type of 3D printing known as bioprinting, researchers combined trophoblast cells with a synthetic gel to create organoids. The cells were deposited in precise droplets, akin to an ink-jet printer, allowing for more accurate positioning. This method resulted in organoids that closely resembled human placental tissue and displayed differences in development compared to those grown in animal-derived gels.
The precise control offered by bioprinting has revealed that the growth environment significantly influences how organoids mature. By adjusting the conditions under which these organoids are cultivated, researchers can better mimic the dynamic environment of the placenta, paving the way for enhanced studies on early pregnancy complications.
The implications of this research are profound. Currently, over 260,000 maternal deaths occur annually due to pregnancy complications, with preeclampsia affecting 5–8% of pregnancies. This condition can lead to severe health risks for both mothers and infants, including organ damage and premature delivery. Understanding the mechanisms behind placental dysfunction is crucial for developing effective preventive measures and treatments.
Future Directions in Placental Research
With the introduction of these bioprinted organoids, researchers can explore the underlying causes of preeclampsia more safely and effectively. For instance, the team exposed the organoids to immune signals prevalent in women with this condition to observe their growth responses. This approach could ultimately lead to the discovery of new therapeutic options.
Furthermore, as the research advances, scientists hope to employ techniques such as CRISPR gene editing to uncover additional factors influencing placental health. Bioprinting not only enhances the accuracy and repeatability of experiments but also aims to reduce reliance on animal models in research, contributing to a more ethical approach in scientific inquiry.
As these models refine, the potential to predict, prevent, and treat serious pregnancy complications could transform maternal healthcare, significantly reducing risks to both mothers and their babies. This innovative work, led by researchers including Claire Richards and Lana McClements, underscores the critical need for continued investment in reproductive health research.
The development of 3D-printed mini-placentas marks a significant step forward in understanding pregnancy dynamics, offering hope for improved outcomes in maternal and infant health worldwide.






