A groundbreaking study has revealed a new electrical signature associated with Parkinson’s disease, shedding light on the neural mechanisms underlying its symptoms. Researchers from the Max Planck Institute for Human Cognitive and Brain Sciences, in collaboration with several leading European institutions, have identified a previously overlooked aspect of brain activity that could lead to more effective treatments for patients with this debilitating condition.
Deep Brain Stimulation Provides New Insights
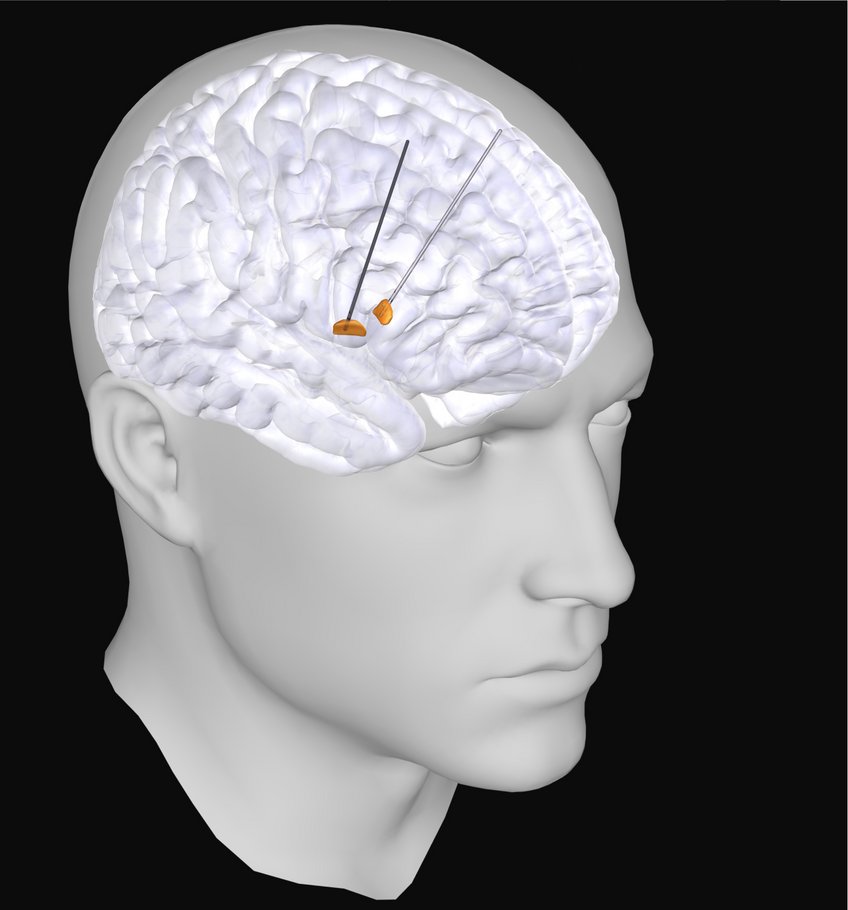
Parkinson’s disease is characterized by movement symptoms that significantly impair quality of life. To better understand what occurs in the brain during these symptoms, scientists are employing various methods, including deep brain stimulation (DBS). This therapy involves implanting electrodes in the brain to alleviate symptoms through electrical impulses. Notably, these electrodes also allow for unique electrical measurements from regions of the brain that are otherwise inaccessible.
With support from the German Research Foundation, the researchers initiated a collaboration involving renowned institutions such as Charité Berlin, Heinrich-Heine University Düsseldorf, University College London, and University of Oxford. They aimed to address inconsistencies found in previous studies regarding the relationship between brain activity and Parkinson’s symptoms, particularly focusing on beta waves, which oscillate approximately 20 times per second.
According to Vadim Nikulin, a researcher at the Max Planck Institute, past studies yielded mixed results, raising questions about whether variations in patient groups, equipment, or analysis methods contributed to these discrepancies. The team sought to find clarity by aggregating several independent datasets and developing a uniform analysis approach.
Key Findings and Implications for Therapy
The findings revealed that the differences in equipment or analysis methods were minimal; rather, sample size emerged as the critical factor. Reliable detection of the correlation between beta waves and symptom severity required data from over 100 patients, while many earlier studies examined significantly smaller cohorts. This new insight emphasizes the need for larger sample sizes in future research.
Additionally, the study highlighted that many previous analyses failed to distinguish between rhythmic and non-rhythmic brain activity, which represent different neuronal processes. Moritz Gerster, who led the study, explained this distinction using the analogy of a concert hall filled with musicians. Some groups create a unified rhythm, while others produce a non-rhythmic noise. Simply measuring the overall volume would obscure these differences.
By utilizing advanced analysis techniques, the researchers successfully separated rhythmic activity from non-rhythmic noise, leading to a clearer understanding of how these patterns relate to patients’ movement symptoms. Furthermore, they found that the anatomical origin of the rhythmic beta waves corresponded more accurately to the most therapeutically effective electrode contact. This discovery could pave the way for automating electrode selection, which currently requires manual expertise.
The clinical diversity among patients posed another challenge for the researchers, as factors such as age, disease duration, and symptom combinations varied widely. With no healthy control group available, the team leveraged a characteristic feature of Parkinson’s disease: its asymmetry. Symptoms often affect one side of the body more than the other, allowing researchers to compare the more-affected hemisphere with the less-affected one.
The analysis indicated that non-rhythmic, noise-like activity was significantly elevated in the more-affected hemisphere, suggesting an increased firing rate of neurons. This finding aligns with observations made in animal models of Parkinson’s disease, as explained by Gerster.
This newly identified electrical signature holds promise for refining deep brain stimulation therapies. Instead of delivering continuous impulses, stimulation could be tailored to match ongoing brain activity, applying treatment only when necessary. The first adaptive stimulators capable of real-time adjustments are already available, paving the way for further exploration of this signature’s effectiveness in everyday conditions.
As follow-up studies commence, researchers are hopeful that this new understanding will contribute to more personalized and effective treatments for individuals living with Parkinson’s disease.