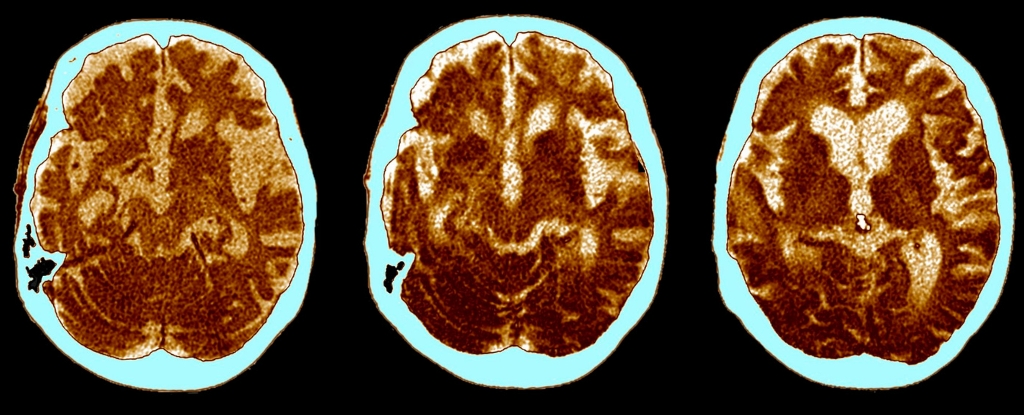
Recent research has uncovered potential benefits of the herpes zoster vaccine, commonly known as the shingles vaccine, beyond its primary purpose of preventing shingles. According to a study published in the journal Nature in April 2025, the vaccine may lower the risk of developing dementia by as much as 20%. This finding could have significant implications for public health, especially as the global population ages and dementia becomes more prevalent.
Vaccines have been instrumental in combating infectious diseases for over two centuries, preventing an estimated 3 million to 5 million deaths each year from illnesses such as diphtheria, tetanus, and influenza, as reported by the World Health Organization. While the primary consensus has focused on their role in infectious disease prevention, this new evidence suggests a broader impact on neurodegenerative disorders.
Research Insights from Wales
The study leveraged a unique opportunity created by a policy change in Wales in 2013, which provided the herpes zoster vaccination to individuals born on or after September 2, 1933. Those born before this date were not eligible for the vaccine, allowing researchers to compare health outcomes between vaccinated and unvaccinated populations without ethical complications.
During a seven-year follow-up period, the research team found that individuals who received the shingles vaccine had a 20% lower chance of developing dementia compared to those who did not. Notably, the data indicated that women experienced a greater benefit than men. This study design enabled a robust analysis without denying vaccination to any participants, as both groups were similarly aged and had comparable medical histories.
The implications of these findings extend beyond the immediate health benefits of vaccination. They suggest a potential role for vaccines in preventing or delaying the onset of dementia, contributing to a growing body of research exploring the intersection of immunology and neurodegeneration.
Understanding the Mechanisms
The mechanisms behind the shingles vaccine’s protective effect against dementia remain to be fully understood. One hypothesis suggests that by protecting against the shingles virus, the vaccine may mitigate factors that exacerbate dementia. Alternatively, the vaccine might enhance the immune system’s overall strength, a phenomenon known as “trained immunity.”
While the study did not differentiate between specific dementia types, such as Alzheimer’s disease or vascular dementia, it raises important questions regarding the protective capabilities of vaccines. The researchers acknowledge the necessity of a prospective, randomized, double-blind, placebo-controlled study—considered the gold standard in clinical trials—to further investigate how the herpes zoster vaccine influences dementia risk over time.
Dementia is a significant global health challenge, with a January 2025 study estimating that individuals aged 55 and older have a 42% lifetime risk of developing the condition. This risk rises dramatically with age, reaching 20% by age 85. Current projections indicate that the number of new dementia cases in the United States could double from approximately 514,000 in 2020 to over 1 million by 2060.
As awareness of dementia’s impact grows, the scientific community is shifting focus to explore innovative therapeutic avenues. Traditional approaches have largely centered on the amyloid hypothesis, which suggests that the accumulation of amyloid protein in the brain contributes to Alzheimer’s disease. Despite significant investment, recent amyloid-lowering therapies have yielded limited success and often come with substantial costs and side effects.
In contrast, studies indicate that routinely administered vaccines could potentially reduce dementia risk. Past research has linked viral exposure to heightened dementia risk, while vaccines against various diseases appear to offer protective benefits.
The exploration of vaccines as a preventive measure for dementia represents a shift in understanding neurodegenerative disorders. As researchers like Anand Kumar and Jalees Rehman from the University of Illinois Chicago emphasize, the scientific community must remain open to new insights, even if they challenge established paradigms.
In conclusion, the potential link between the shingles vaccine and reduced dementia risk is a promising development in the ongoing battle against neurodegenerative diseases. As further studies are undertaken, the possibility that vaccines may play a crucial role in dementia prevention opens exciting new avenues for research and public health strategies.