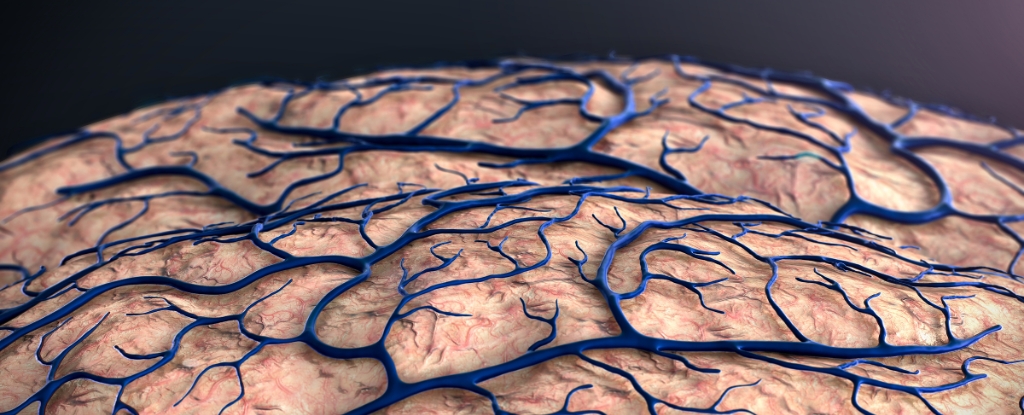
Research into the onset of Alzheimer’s disease has taken a significant turn, with new findings indicating that the disease may start at the brain’s protective borders rather than within its core. Scientists from the United States and Germany have linked genetic risks for Alzheimer’s and other neurological disorders to the blood-brain barrier, the network of blood vessels and immune cells that safeguard the brain.
Traditionally, studies have concentrated on the abnormal protein clumps and tangles within the brain that damage neurons. However, this latest research suggests that the initial triggers of Alzheimer’s could stem from external factors breaching a compromised brain boundary.
Neuroscientist Andrew Yang from the Gladstone Institute of Neurological Disease in California emphasized, “When studying diseases affecting the brain, most research has focused on its resident neurons. I hope our findings lead to more interest in the cells forming the brain’s borders, which might actually take center stage in diseases like Alzheimer’s.”
The research team developed an innovative genetic analysis technique called MultiVINE-seq. This method allows researchers to isolate vascular and immune cells from brain tissue, measuring their gene activity and chromatin accessibility, which relates to how readily DNA can be utilized by cells. Analyzing 30 postmortem brain tissue samples from individuals with and without neurological disease, the scientists constructed a detailed profile of genetic variations associated with conditions like Alzheimer’s.
Many of the genetic variations identified were located in cells patrolling the brain’s borders, particularly in endothelial cells, which regulate access to the brain, and T cells, part of the immune system. Certain genetic variants implied that inflammatory immune cells could be instigating or accelerating the onset of Alzheimer’s.
Neuroscientist Madigan Reid, also from the Gladstone Institute, noted, “Before this, we knew these genetic variants increased disease risk, but we didn’t know where or how they acted in the context of brain barrier cell types. Our study shows that many of the variants are actually functioning in blood vessels and immune cells in the brain.”
Understanding neurodegenerative diseases like Alzheimer’s is complex, influenced by numerous factors, which often slows progress in treatment development. Nonetheless, this study advances knowledge about how these diseases operate and highlights the importance of the brain’s vascular and immune systems.
Previous research has already established links between Alzheimer’s disease and broader immune system issues, extending beyond the brain itself. This latest study also revealed that different genetic risk variants exert varying effects on the brain’s borders, depending on the disease, paving the way for tailored treatment approaches.
“This work brings the brain’s vascular and immune cells into the spotlight,” Yang stated. “Given their unique location and role in establishing the brain’s relationship with the body and outside world, our work could inform new, more accessible drug targets and lifestyle interventions to protect the brain from the outside in.”
The findings were published in the journal Neuron, marking a pivotal step toward a deeper understanding of Alzheimer’s disease and its origins.