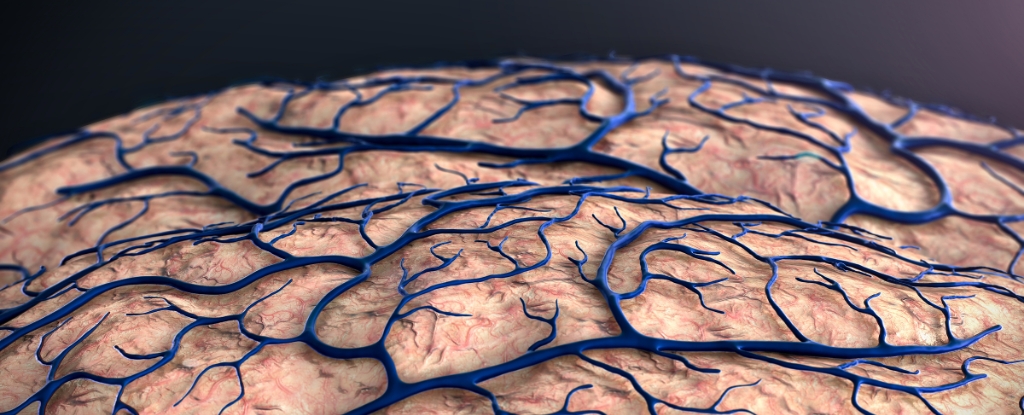
Research from scientists in the United States and Germany has unveiled new insights into the origins of Alzheimer’s disease, suggesting that the initial triggers may lie at the brain’s borders rather than within its core. This study highlights the role of the blood-brain barrier, which consists of blood vessels and immune cells that protect the brain, in the disease’s onset.
Traditionally, Alzheimer’s research has focused on the protein clumps and tangles that damage neurons inside the brain. However, the findings from the Gladstone Institute of Neurological Disease indicate that compromised barriers could allow harmful intruders to enter and initiate the disease. Neuroscientist Andrew Yang emphasizes this shift in focus, stating, “When studying diseases affecting the brain, most research has focused on its resident neurons. I hope our findings lead to more interest in the cells forming the brain’s borders, which might actually take center stage in diseases like Alzheimer’s.”
This research builds on previous genetic studies that have shown variations in DNA sequences associated with neurological conditions often occur in regulatory regions outside of protein-coding genes. These regions play a crucial role in fine-tuning gene expression and controlling cellular activity.
Innovative Genetic Analysis Technology
The research team developed a new technology called MultiVINE-seq, which isolates vascular and immune cells from brain tissue. This method allows scientists to measure gene activity and chromatin accessibility, providing a layered understanding of genetic variations that are linked to Alzheimer’s and other brain diseases. The team analyzed 30 postmortem brain tissue samples from individuals with and without neurological diseases, uncovering significant patterns.
Their findings revealed that many genetic variations are associated with endothelial cells, which regulate access to the brain, and T cells, key players in the immune response. Notably, certain genetic variants suggested that inflammatory immune cells could potentially trigger or accelerate Alzheimer’s. “Before this, we knew these genetic variants increased disease risk, but we didn’t know where or how they acted in the context of brain barrier cell types,” said Madigan Reid, another neuroscientist at the Gladstone Institute.
Understanding Complex Neurodegenerative Diseases
Neurodegenerative diseases like Alzheimer’s are complex, influenced by multiple factors, which makes progress toward effective treatments slow. Nevertheless, this study adds a vital piece to the puzzle, enhancing our understanding of how diseases originate.
Previous research has also connected Alzheimer’s to broader immune system issues beyond the brain. The current study further suggests that different genetic risk variants affect the brain’s borders in unique ways depending on the specific disease. This information could provide critical insights into developing targeted treatments.
Yang concluded, “This work brings the brain’s vascular and immune cells into the spotlight. Given their unique location and role in establishing the brain’s relationship with the body and outside world, our work could inform new, more accessible drug targets and lifestyle interventions to protect the brain from the outside in.”
The findings were published in the journal Neuron, marking an important step forward in Alzheimer’s research and offering hope for future treatments.







