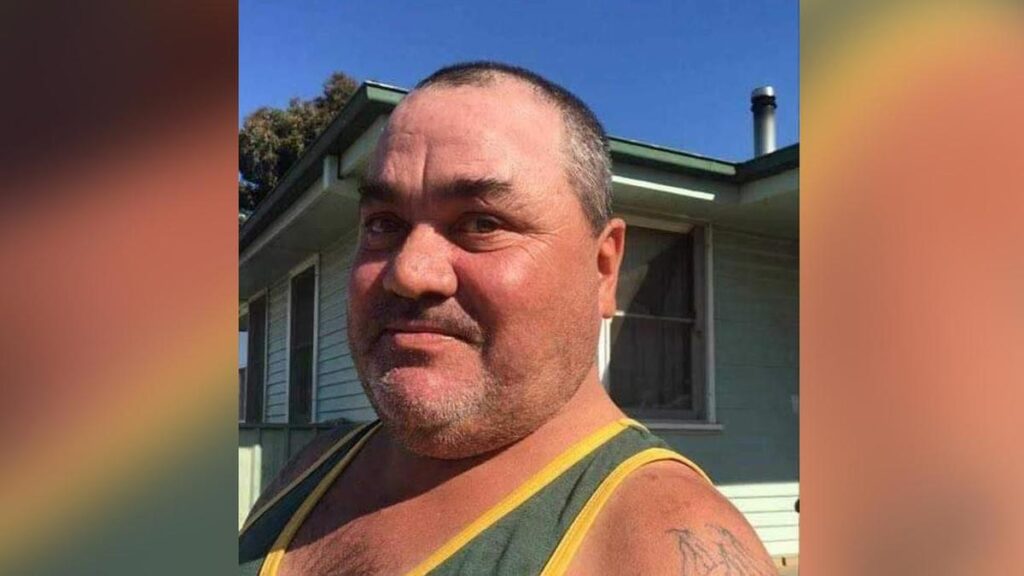
A coroner’s inquest has concluded that a father of five, Paul Harris, should have received specialized care before his death from complications related to Q fever and a blood clot that went undiagnosed at a small rural hospital. Mr. Harris passed away at Hay District Hospital in New South Wales on October 17, 2019, after initially being treated for what was suspected to be community-acquired pneumonia.
The inquest revealed that the 43-year-old Indigenous meat worker had been admitted to the hospital in late September 2019 with pneumonia and was discharged after responding to antibiotic treatment. However, on October 9, he returned to the medical center complaining of coughing up blood. A doctor who worked in both the clinic and the hospital re-admitted him, initially considering the possibility of a lung clot.
Despite the doctor’s concerns, further examinations led to a belief that recurrent pneumonia was the more likely diagnosis. The doctor did not test for Q fever, assuming that the antibiotics prescribed for pneumonia would also address the underlying infection.
As Mr. Harris’s condition failed to improve over the following days, the doctor ordered additional tests but did not transfer him to the larger Griffith Hospital for a critical CT angiogram. Expert reports presented during the inquest indicated that his care should have been escalated, as the two doctors at Hay Hospital relied on “most likely” scenarios instead of ruling out more serious conditions.
Deputy State Coroner Rebecca Hosking determined that Mr. Harris should have been transferred to Griffith Hospital for further examination. Although she acknowledged that the antibiotics for pneumonia would have treated both conditions, she could not definitively conclude whether earlier detection of the blood clot could have saved his life.
The inquest also highlighted that Mr. Harris’s job at a kangaroo meat processing facility put him at higher risk for Q fever, which should have been identified sooner. While evidence presented pointed to a link between Q fever and blood clots, this connection is not widely recognized among healthcare professionals.
In her findings, Ms. Hosking expressed her condolences to Mr. Harris’s family, describing him as a cherished father and step-father to five adult children. “He had a big personality and was described by his family as a larrikin, who enjoyed making people laugh,” she stated in Lidcombe Coroners Court. The family continues to feel the profound loss of a man who was integral in their lives, particularly during significant milestones.
As a response to the findings, Ms. Hosking recommended that the Murrumbidgee Local Health District implement training for its staff to foster better relationships between hospitals in the region. The aim is to enhance patient care and ensure that similar oversights do not occur in the future.
The tragic case of Paul Harris underscores the critical importance of thorough medical assessments in rural healthcare settings, particularly when patients present with complex symptoms.






