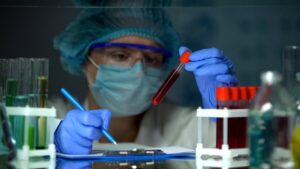
URGENT UPDATE: Australia is confronting an alarming rise in sexually transmitted infections (STIs), with experts urging immediate action to combat this public health crisis. New data reveals that in 2024, the country recorded nearly 6,000 diagnoses of syphilis and more than 44,000 cases of gonorrhoea, doubling the rate of reported infections over the last decade.
The situation is particularly dire for chlamydia, which remains the most frequently reported STI with over 100,000 diagnoses in 2024. The majority of these cases, approximately half, were among individuals aged 20 to 29 years. Alarmingly, a recent analysis by the Kirby Institute indicates that only 16 percent of Australians aged 16 to 49 have ever been tested for STIs, highlighting significant gaps in sexual health awareness and care.
Dr. Skye McGregor, an epidemiologist, warns, “Chlamydia, gonorrhoea, and syphilis are bacterial infections that can usually be easily treated and cured with antibiotics. However, if left untreated, STIs can cause serious long-term health concerns like pelvic inflammatory disease and infertility in women.”
Experts are particularly concerned about the rising syphilis rates among women of child-bearing age. If not treated during pregnancy, syphilis can lead to devastating outcomes including miscarriage, stillbirth, or congenital syphilis, where the infection is passed on to the unborn child. Since 2015, cases of congenital syphilis have more than doubled, resulting in 34 infant deaths in the past decade, with over half of these tragic cases occurring among First Nations Australians.
“The impact of congenital syphilis is severe, resulting in significant lifelong health issues for infants, and in the most severe cases, can be fatal,” Dr. McGregor added.
Indigenous Australians face disproportionately high rates of STIs, with chlamydia diagnosed at more than twice the rate, gonorrhoea almost four times higher, and syphilis more than five times higher compared to non-Indigenous populations. Robert Monaghan, manager of the Yandamanjang First Nations Health Research Program, emphasized the need for culturally safe, community-led initiatives to effectively address these sexual health gaps.
Stigma surrounding STIs, particularly HIV, remains a significant barrier to public health. Dr. McGregor highlighted the necessity of normalizing discussions about sexual health, urging individuals to engage openly with new and regular partners, as well as healthcare providers.
In 2024, there were 757 new HIV diagnoses, marking a 27 percent decline from the previous decade. Of these, over 60 percent were attributed to sex between men, while 27 percent were linked to heterosexual sex and 3 percent to injecting drug use.
Scott Harlum, president of the National Association of People with HIV Australia, stressed the importance of recognizing the human stories behind each diagnosis: “While the numbers reflect a decline, we must do much more to achieve the goal of virtually eliminating domestic HIV transmissions in Australia by 2030. Each person diagnosed has a lived experience that sheds light on the systemic failures in preventing HIV transmission.”
This developing situation calls for urgent attention and action from both health authorities and the public. Empowering individuals with the knowledge and resources to seek regular testing and treatment is crucial in reversing the concerning trends in STIs.
WHAT’S NEXT: Health officials are expected to announce new initiatives aimed at increasing awareness and accessibility of STI testing across Australia. As the crisis unfolds, communities are urged to engage in dialogues about sexual health to combat stigma and promote prevention.